The ATMP research and development lifecycle
Advanced Therapy Medicinal Products (ATMPs) are highly innovative technologies, based on gene transfer or cell/tissue engineering, that can provide long-lasting and potentially curative benefits for patients suffering from rare and other chronically debilitating diseases, often by targeting the root cause of these conditions.1 A dynamic life sciences ecosystem in the EU brings these cutting-edge technologies to patients, with over 220 European universities/public institutions involved in their development and a further 359 private developers engaged across the sector in the EU.2
The development of new ATMPs, from target discovery to market approval, can take as long as 15 years3, and often involves a wide range of partners, each contributing in a unique and indispensable way. In order to ensure the fastest patient access possible, we need to leverage tools, such as horizon scanning, that anticipate health technology advances and help lay the groundwork for sustainable uptake by national healthcare systems.
Scroll down to find out more about each stage of the lifecycle.







The drug development process begins by understanding the biological mechanism(s) that lead to a disease. The mechanism in question may involve a target like an enzyme or a gene. Researchers then explore a range of compounds, looking for possible interactions with the biological target that are expected to limit or cure the associated condition. In the case of rare diseases, the often more limited understanding of the underlying biology makes this basic and translational research more challenging, as it often requires researchers to explore uncharted territory in researching new biological targets. In addition, ATMP development often relies on innovative technologies, such as gene editing and cell engineering, that add complexity to this stage of the research and development (R&D) process. The time and financial investment needed by basic research and early discovery can therefore be significant.
At this point, most of the compounds explored will be unsuccessful, meaning this stage of R&D is associated with significant risk and uncertainty.4
Given the risk and large investments needed in basic and translational research, multistakeholder collaboration is especially important at this stage. Regulatory and financial support from public authorities, and collaboration with non-for-profit or academic researchers, can help support these major undertakings. Importantly, basic research into the genetic and molecular causes of rare and other chronic conditions is associated with significant scientific spillover to other disease areas, advancing care for everyone.
4 Mohs, R. C., & Greig, N. H. 2017. Drug discovery and development: Role of basic biological research. Alzheimer S & Dementia Translational Research & Clinical Interventions, 3(4), 651–657. https://doi.org/10.1016/j.trci.2017.10.005
Before a therapeutic candidate can be tested in human populations through clinical trials, developers must validate the initial toxicologic and pharmacokinetic profile of the candidates. The preclinical stage is therefore another phase in the drug development cycle associated with high costs and risk of failure for most candidates.5
Unlike small molecule drugs, ATMPs act by inserting recombinant genes into cells, or by introducing modified cells or tissues into the body. ATMPs therefore present particular challenges for preclinical investigations: classic approaches to assessing pharmacokinetic properties do not apply to ATMPs, and the translation of relevant findings from animal models to human subjects can be severely limited. In addition, some ATMPs consist of or contain genetically-modified organisms (GMOs), meaning that investigational products must comply with the GMO Regulation requirements on Environmental Risk Assessment before clinical trials can even begin, leading to additional regulatory burden. Similarly, ATMPs containing a medical device as an integral part of the therapy require safety data to be provided for the device as well, ahead of clinical trials.
5 Zurdo, J. 2013. Developability assessment as an early de-risking tool for biopharmaceutical development. Pharmaceutical Bioprocessing, 1(1), 29–50. https://doi.org/10.4155/pbp.13.3
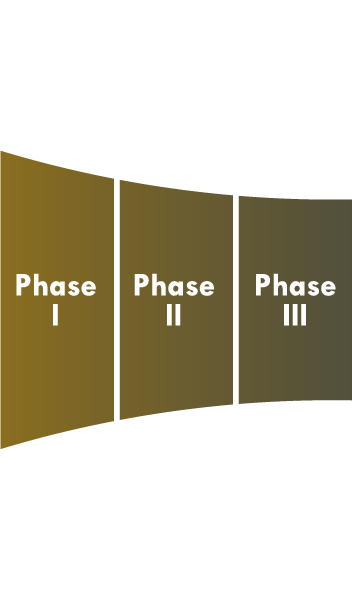
Clinical trials have three phases:
Phase I confirms if the potential therapy is safe (and at what dosage) for humans, using a small sample of individuals.
Phase II involves a larger sample size, to assess the impact of the treatment across key biomarkers.
Phase III tests the relative efficacy of the therapeutic candidate compared to other available therapies – if any – in an even larger sample of individuals.
Designing clinical trials for investigational ATMPs is more difficult compared to traditional therapies. There are ethical barriers to applying standard clinical trial templates to ATMPs: for example, because of the higher risk associated with giving healthy volunteers a gene therapy, the safety profile is validated using patients instead of healthy volunteers, making the interpretation of the safety data more difficult; the use of standard trial templates, such as large double-blind placebo controlled trials, is especially difficult in the case of ATMPs. In the case of some rare diseases, trial populations will be smaller, harder to identify, and will display very different disease pathologies, adding more difficulty to data interpretation. All these issues mean that ATMP developers face significant challenges and uncertainties in constructing the clinical data dossier for their products.
Finally, because rare disease populations are sparsely distributed across many countries, developers must conduct multi-state clinical trials and face additional regulatory burden: as clinical trials are regulated nationally, developers need to tailor clinical development plans and applications to the regulatory standards of each country.
It is important to note that, as a consequence, the EU’s share of ATMP clinical trials is decreasing: recent numbers show that only 31% of the total pharmaceutical R&D investment effort takes place in the EU, while clinical trial activity for ATMPs is two to three times higher in regions outside the EU, such as the US and China. In 2020 only 19.3% of all clinical trials conducted globally on investigational ATMPs took place in Europe.6
6 Charles River Associates. 2022. Factors affecting the location of biopharmaceutical investments and implications for European policy priorities. Final Report. Prepared for European Federation of Pharmaceutical Industries and Associations (EFPIA). https://www.efpia.eu/media/676753/cra-efpia-investment-location-final-report.pdf
ATMPs obtain EU-level marketing authorisation through the centralised procedure of the European Medicines Agency (EMA). The EMA assesses whether a new therapy is safe and efficacious for treatment of a given condition. Currently, the scientific assessment of ATMPs is conducted by three Committees, of which the Committee for Advanced Therapies (CAT) plays a central role.* The CAT issues the first opinion on every application, gives recommendations on ATMP classification, and offers scientific advice and expertise on initiatives contributing to ATMP uptake in drug development pipelines.
Many currently authorised ATMPs are registered orphan medicinal products (OMPs) or address an unmet need, benefitting from the regulatory incentives associated with these designations: scientific advice and early communication with EU regulators through PRIME, and with payers and HTA agencies at the national level, can enhance the quality of the clinical trial designs and data collection, mitigating some of the uncertainties and risks associated with ATMP research and development and greatly increasing the likelihood of regulatory approval and reimbursement. Conditional marketing authorisation or approval under exceptional circumstances can fast-track the regulatory process, with the aim to increase the speed with which innovative therapies reach patients.
* The EMA committee structure is currently being revisited under the revision of the General Pharmaceutical Legislation: the proposal would see some of the current committees – including CAT – disbanded and their activity replaced by working groups.
One of the most difficult stages in the ATMP journey to patient access covers national-level pricing and reimbursement (P&R). Health technology assessment (HTA) assesses the value of a new therapy to the healthcare system. Because most ATMPs are intended to be one-off treatments, data about these therapies’ long-term cost-effectiveness and therapeutic added value are more difficult to obtain prior to authorisation and routine administration.7 Hence, it is important that these therapies benefit from support beyond regulatory approval and into market access if timely patient delivery is to be achieved: if an ATMP can be granted (conditional) marketing authorization by the EMA on the basis of early or incomplete safety and efficacy data, measures must be taken to ensure efficiency at the P&R stage as well, since often the type of data required by traditional HTA instruments cannot be generated in a timely fashion by ATMP developers. This can contribute to significant delays to patient access and the administration of ATMPs outside clinical trials and early access programmes.
To overcome these limitations, there is great need for better alignment among regulators and national HTA and payer authorities on the requirements for ATMP clinical data portfolios, as well as for improved dialogue and support for developers in the form of consolidated scientific advice and guidelines. Additionally, duplication of evaluation efforts at the EU and national levels should be avoided. The HTA Regulation, which applies to ATMPs as of January 2025, is expected to reduce duplication by requiring joint clinical assessments at the EU level, but significant uncertainties regarding the process still remain. Finally, novel payment mechanisms, such as outcome-based agreements, should be designed and implemented to support the collection of real world evidence (RWE) on ATMP safety and efficacy.
7 Rejon-Parrilla, J. C., Espin, J., Garner, S., Kniazkov, S., & Epstein, D. 2023. Pricing and reimbursement mechanisms for advanced therapy medicinal products in 20 countries. Frontiers in Pharmacology, 14. https://doi.org/10.3389/fphar.2023.1199500
Phase IV is an additional stage of the drug development process. Therapies that receive conditional marketing authorisation must complete ongoing clinical studies or start new ones to collect additional data confirming the therapy’s efficacy and risk-benefit balance. Regulators might also require Phase IV data collection to validate the long-term safety profile of the product and monitor for unexpected side effects. For ATMPs, and especially gene replacement therapies, this stage is especially important since their mode of action opens specific pharmacovigilance questions regarding insertional mutagenesis, viral latency/reactivation, toxicity, and accuracy of clinical follow-up. Close monitoring is also recommended with regards to batch characteristics, administration, storage and distribution.8
Phase IV studies offer an important opportunity for developers to reduce uncertainty and strengthen the clinical data portfolio of their products: RWE collected during post-authorisation studies can offer valuable insight into the product’s long-term efficacy while supporting innovative payment and risk-sharing solutions.
8 Petitpain, N., Antoine, M. L., Beurrier, M., Micallef, J., & Fresse, A. (2023). Pharmacovigilance of gene therapy medicinal products. Rare Disease and Orphan Drugs Journal, 2(4). https://doi.org/10.20517/rdodj.2023.19
Many ATMPs, including cell-based gene therapies like CAR T-cell therapies, require specialised technology and know-how for delivery and administration. Newborn screening, an important tool in the timely diagnosis and treatment of conditions affecting children’s long-term health and survival, is similarly constrained by these infrastructural and knowledge gaps. As a consequence, ATMP delivery and newborn screening can often only be done in centres of excellence and by trained healthcare professionals.
The European framework for cross-border healthcare should provide a strong and effective safety net to EU citizens for whom access to ATMPs is severely limited or nonexistent in their own countries. However, several challenges related to payment mechanisms, prior authorisation and knowledge gaps continue to persist. The current Cross-Border Healthcare Directive requires patients to pay in advance for the treatment, which poses significant obstacles to equitable patient access. Moreover, the ‘home’ Member State can decide on a case-by-case basis which treatments are deemed required or available to the patient. An equally important issue concerns the knowledge gaps of medical professionals and their patients, who might not be aware of treatment options involving ATMPs or patients’ rights to health services abroad. In the case of rare diseases, involving to a greater extent European Reference Networks and facilitating patient access to National Contact Points could help overcome some of these challenges.
Horgan D, Metspalu A, Ouillade MC, Athanasiou D, Pasi J, Adjali O, Harrison P, Hermans C, Codacci-Pisanelli G, Koeva J, Szucs T, Cursaru V, Belina I, Bernini C, Zhuang S, McMahon S, Toncheva D, Thum T. 2020. Propelling Healthcare with Advanced Therapy Medicinal Products: A Policy Discussion. Biomed Hub. 3;5(3):130-152. doi: 10.1159/000511678. PMID: 33987187; PMCID: PMC8101061.
Alliance for Regenerative Medicines. 2024. Cell and Gene Therapy Sector Data: Q2 2024: Therapeutic Developers. https://alliancerm.org/data/
Singh, N., Vayer, P., Tanwar, S., Poyet, J., Tsaioun, K., & Villoutreix, B. O. 2023. Drug discovery and development: introduction to the general public and patient groups. Frontiers in Drug Discovery, 3. https://doi.org/10.3389/fddsv.2023.1201419